Minnesota: The Great Poisoning
"We Need To Talk About Kidney"
Introduction
Back when I started analyzing spontaneous adverse event reports, I noticed a safety signal for Acute Kidney Injury in the VAERS reports.
This signal is weaker when excluding reports about COVID cases:
…and shockingly strong when restricting the analysis to reports about COVID cases:
While never really putting much thought into this, I did mention the signal in a few articles. The best explanation I had was “infection enhancement”, since we can see a very similar pattern in a number of other symptoms.
When I started analyzing the public US data provided by the CDC I noticed kidney deaths had been on the rise since early 2020, but particularly since introduction of the vaccines, so I prepared to write an article about it.
Alas I found no correlation between vaccination rates and increases in kidney deaths, figured it might just be COVID-19 itself and scrapped the idea of writing about it. There were after all plenty of online articles - a lot of them published in once respected journals - claiming SARS-CoV-2 was a major cause for acute kidney injuries.
I don’t remember who pointed it out, but recently someone somewhere said something along the lines of “Isn’t it odd that a respiratory pathogen would be causing kidney injury?”
That is indeed very odd. It should have been obvious. I don’t know why it took so long for me to realize this.
Increases In Kidney Deaths
With the US government - like many other governments - having the habit of suppressing deaths for privacy reasons when the death count in a certain subpopulation/region/timeframe is 1-9, most of the data that can be acquired from public datasets or via CDC Wonder is plain useless.
Fortunately I recently acquired 8 years of Minnesota death certificates, which we can now use to look into what might be causing these kidney deaths. I too will suppress data whenever it is appropriate, but only then.
There are three diagnostic groups in ICD-10 related to renal pathologies (N17-N19), so let’s first look at all three separately.
Unspecified kidney failures have been declining since 2015, but acute kidney failures and chronic kidney injuries are clearly seeing some unusual action in the past few years.
To get a better picture of these developments, I will calculate an excess series from each timeseries. To do this, I will:
Remove linear trends by…
determining the linear trend between 2015 and 2019
correcting the entire timeseries for this trend, leaving the most recent week untouched
Remove seasonality by…
comparing each weekly figure with the respective calendar week’s average throughout 2015-2019.
These are deaths after trend correction. It now seems there is actually a little something going on with N19 as well. Let’s look at the excess series, absolute and relative.
For the absolute excess series I am subtracting the historical averages from the current values. This retains information about the number of deaths.
For the relative excess series I am dividing the current values by the historical averages. This swallows information about the number of deaths, but allows for a more direct comparison of trends.
Absolute Excess Kidney Deaths
Chronic Kidney Disease And COVID-19
The above chart is highly informative. Look at the blue line that represents all decedents whose death certificates mentioned chronic kidney disease.
According to this article SARS-CoV-2 doesn’t like patients with chronic kidney issues. It is considered a high-impact comorbidity which makes infected individuals more susceptible to COVID death by a factor of 4.3 (95% CI 3.6–5.3).
Please excuse the scaling in this one. I hope you get the idea. Excess deaths of (very expensive) kidney patients co-occurred with COVID waves and were almost exclusively associated with COVID-19 diagnoses.
Throughout 2022 there a mortality deficit manifested in these kidney patients, so I can only assume that COVID-19 provided some long-needed relief for our healthcare and pension systems.
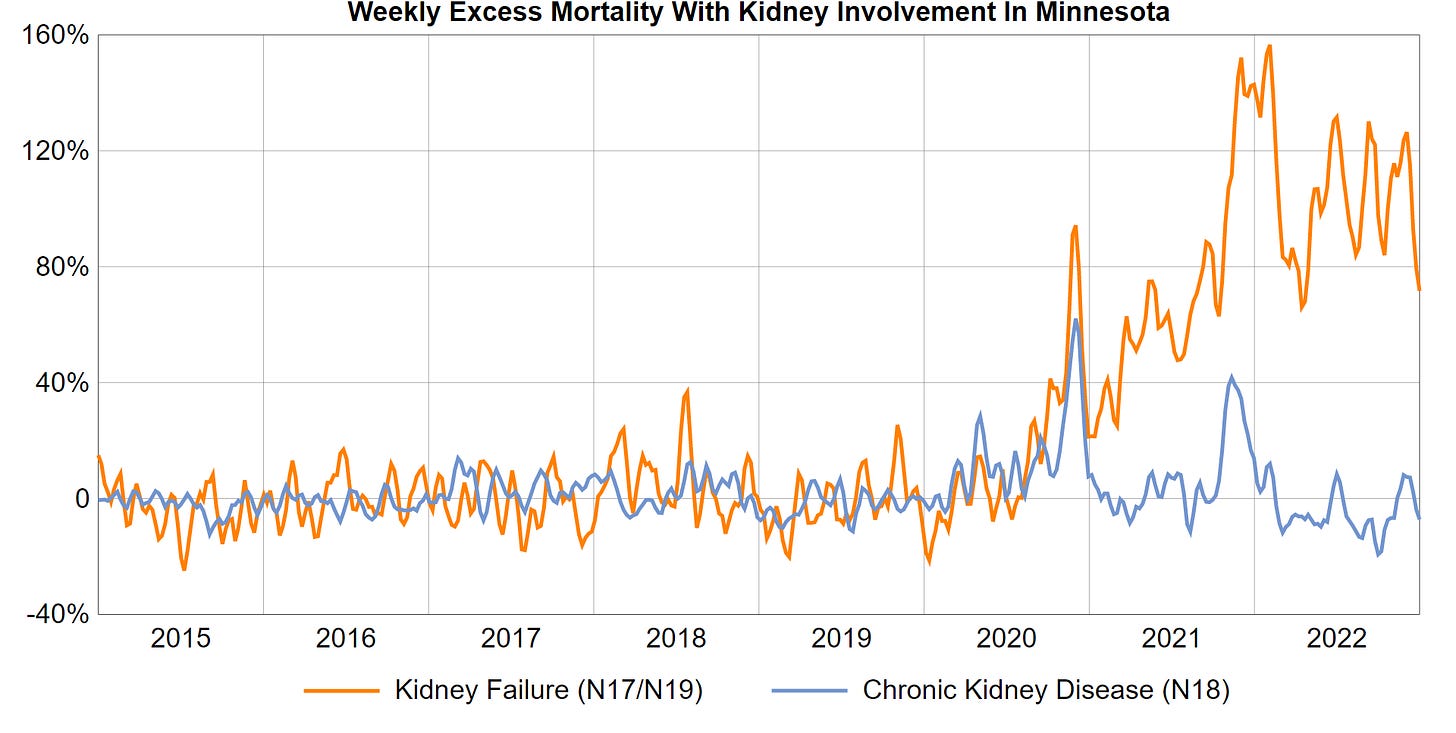
Let’s look at relative excess deaths now.
Relative Excess Kidney Deaths
This is a bit hard to read. Let’s group N19 and N17 into “Kidney Failure (N17/N19)”.
Not much to be said here at this point. I intend to track these deaths down.
Kidney Failures In And Outside Of Hospitals
I am separating kidney failure deaths into two categories:
Kidney failure deaths occurring inside hospitals
Kidney failure deaths occurring outside of hospitals
I will apply the same techniques to calculate excess series for both categories.
Here are the same variables for nursing homes instead of hospitals
So whatever happened, it is safe to say it happened in hospitals, but not in care homes.
While this is not the focus of the article, do take note of the nursing home mortality deficit we are seeing all throughout 2021 and 2022. The sickly are gone. They are no more a burden to us like we once were a burden to them, when they invested their life force into raising us to the utilitarian monsters we have become.
But I digress. We tracked the almost constant rise in kidney failures we have been seeing in Minnesota since mid-2020 to hospitals.
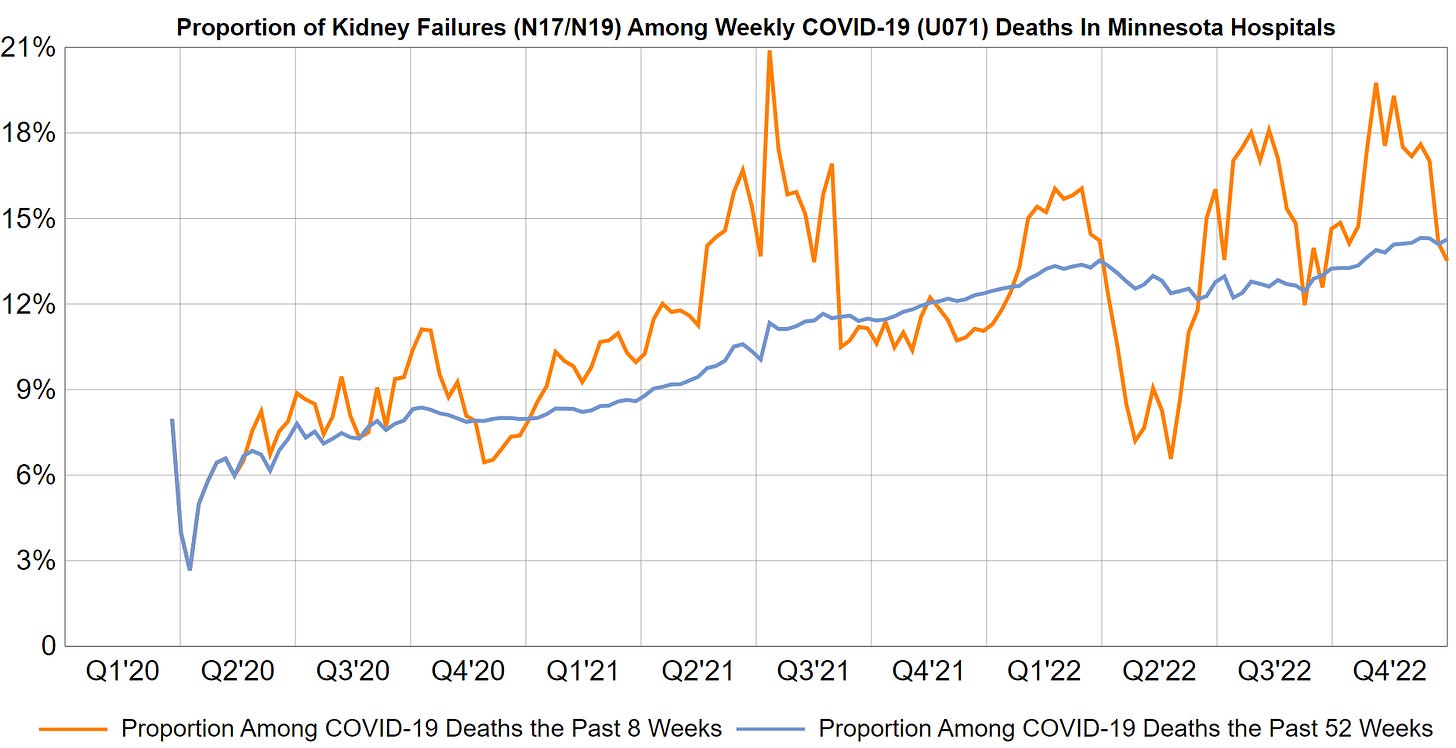
Kidney Failure in COVID Patients
Next, we will look at how the proportion of kidney failures in hospitalized COVID-19 decedents changed over time.
If COVID was to blame for kidney injuries, I would expect the proportion of COVID deaths to…
either be constant
or declining, since…
those most susceptible to such complications would be eradicated throughout the course of a pandemic
disease management will improve as we gather more data
The blue line is a moving average with a period of 52 weeks and tells us that the proportion of COVID decedents with acute renal failure increased from 8% throughout 2020 to 14% throughout 2022, which is a 75% relative increase.
Since a number of experimental pharmacotherapies were being deployed by April 2020, it is not entirely unlikely that the relative increase compared to deploying no such experimental interventions is far north of 75%. Alas we just don’t have such reference data, because this is how COVID-19 began - with global top-down medical interventions.
We can look at these deaths in some more detail yet. So let’s zoom in.
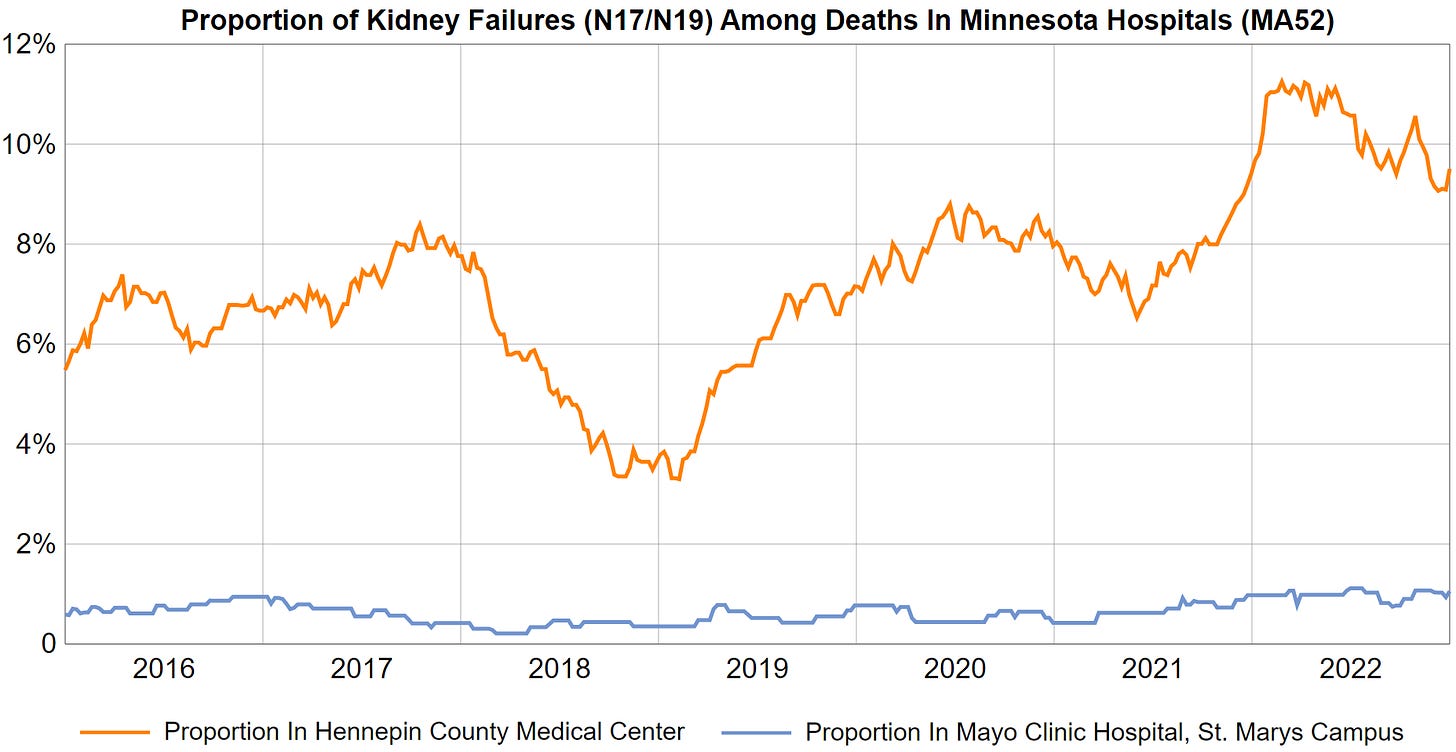
Are All Hospitals Affected?
I have already prepared a spreadsheet with an overview of all Minnesota hospitals, which I then reduced to a short list containing just a few of of the biggest and most remarkable clinics. I also prepared six charts that include N19 on top of acute kidney injuries (N17).
The y-scaling is the same for all hospitals.
This is where things get weird.
The Mayo Clinic in Rochester - arguably one of the best hospitals in the USA - has not seen a single one of their COVID-19 patients die after suffering acute kidney failure.
The Abbot Northwestern Hospital - belonging to Allina Health which are among the biggest pandemic losers in terms of changes in net income - only saw 2.0% (95% CI: 1.0%-3.6%) of their COVID decedents suffer acute kidney failure.
The other four clinics saw whopping rates of around 15% of their COVID-19 decedents suffering acute kidney failure.
What I feel confident enough to say at this point is:
Most deaths due to acute kidney failure in COVID-19 patients are avoidable.
This does not mean that acute kidney failure is avoidable altogether in COVID-19 patients, but deaths resulting from it apparently are. Otherwise we would be seeing them in all clinics.
I checked each of these hospitals for the existence of nephrology departments. It seems the only one lacking those are Regions Hospital and St. Cloud Hospital. Coincidentally these are the two hospitals in our list with the most COVID deaths per staffed bed.
It would be nice to see the total number of monthly COVID cases registered in each hospital to get an idea of the respective CFR’s, but I do not have any such data at my disposal. What we do have are the number of COVID deaths per bed, but we should not rely on that variable.
It is safe to assume that quality of care is one of the most critical aspects when it comes to COVID outcomes though.
The Mayo Clinic takes medicine very seriously, as can be gathered from their track record and some of the writings I found on their website:
Some excellent critical thinking demonstrated in their Vitamin D recommendations
A clinical trial looking at 1-year survival rates of COVID-19 patients with and without AKI
Because it will ultimately not be possible to pin these deaths to specific aspects of treatment based on death certificates alone, I decided to ask Kai Singbartl MD from the Mayo Clinic in Rochester for some insights:
Since he is unlikely to reply in the next few minutes - and not very likely to reply at all - I am going to have to gather some more data myself.
Out of curiosity I wanted to see the rates of patients with chronic kidney disease among the COVID decedents, so I prepared another table and a few charts. I also included the number of patients who were affected by both chronic kidney disease (N18, CKD) and kidney failure (N17/N19, KI).
While Mayo Clinic and Abbot Northwestern Hospital are again seeing the lowest rates among their COVID decedents, all hospitals are in a much more narrow range now. Other than that there is not much to see here.
I want to find out why we are seeing such large differences in the rates of kidney failures among COVID-19 decedents between hospitals.
There needs to be an explanation.
Remdesivir Trials
When I started writing this article, I had already made up my mind. Remdesivir must be the sole culprit for millions of kidney failures worldwide.
I had created this chart and was just looking for more evidence.
But I’m afraid things aren’t quite that simple.
Remdesivir Trial Participation
So with Remdesivir as the main suspect, I wanted to find out which of the clinics participated in the trials in early 2020. Maybe I would find particularly high rates of kidney failure among them.
So I queried the CMS OpenPayments database to find out which hospitals in Minnesota participated in the Remdesivir trials.
These are the summarized results:
The two largest clusters of grants were paid to the Hennepin County Medical Center and the Mayo Clinic in Rochester.
And this is where the narrative crumbles. If it is as simple as “Remdesivir is killing all these people”, we would not be seeing such low rates of kidney failure deaths in the Mayo Clinic:
GS-US-540-5773 is the study in which 5-day and 10-day treatment plan were compared, without any type of control group. Just through and through horrible study design that only serves to deceive.
But what we can extract from this is that Mayo Clinic patients must have actually received the drug. Well only 5 of the 73 trial sites were FDA-inspected, but I suppose we can take it in good faith that the Mayo Clinic did administer the drug.
We have to ask ourselves why there were no COVID deaths with acute kidney failure in the Mayo Clinic, because Remdesivir is most definitely nephrotoxic:
I don’t have the original data, so I can’t calculate confidence intervals, but by now there are mountains of evidence that Remdesivir can cause kidney injury. Nobody denies it, so I’ll spare you with the evidence.
The drug was not given to patients with chronic kidney disease until GS-US-540-9015, the single dose trial in patients with kidney disease which results came in in late November 2022.
Yes you read correctly. A single dose trial that was completed more than 2.5 years after we had begun shooting this stuff into every other COVID patient and his dog. It’s the one Daniel K. Ries raked in 300k for (see payments table above), before the shady-ass company that seems to have conducted this trial in Minnesota was renamed from “Prism Research” to “Nucleus Network Minneapolis”.
Let’s not go down this road. The trials are flat-out shady, deceptive, plain ridiculous. Nobody who is interested in actually acquiring information about the efficacy and safety of a substance would ever design them the way they were designed, but it would be very tedious to get into this.
If you want a summary of all the trials, just ask Gilead. This was just released on May 12, 2023. Here’s their conclusion:
What I was asking myself when I saw the Mayo Clinic participating in GS-US-540-5773 and GS-US-540-5774 is still:
Why were there no kidney failures among Mayo Clinic’s COVID decedents?
When browsing the Mayo Clinic website, I stumbled over a number of internal studies they are conducting on the proper use of Remdesivir.
The Mayo Clinic seems to be aware that the only research you can really rely on is the one you conduct yourself.
Considering that none of their COVID patients died of acute kidney injury despite their use of Remdesivir, the drug probably truly has its place in the treatment of COVID.
Maybe there are other mechanisms at play here.
How Do Kidneys Become Injured?
Chronic kidney disease is most often a result from diabetes, high blood pressure or glumerulonephritis. Glumerulonephritis in turn isn’t really a specific disease, but a pathological process that can arise from countless causes, among them infections, drugs, autoimmunological processes and genetic disposition.
We are only interested in acute kidney injuries though.
What’s important to understand is that roughly 16% of acute kidney injuries are caused by administration of nephrotoxic drugs, while - based on my pre-COVID knowledge - viral infections are not a causative factor that ever even deserved a mention, so let’s pin that to <1%.
If you want to know more about drug-induced nephrotoxicity, this is an excellent article.
Here is an incomplete list of drugs that can give rise to AKI:
When there is a sudden increase in acute kidney injuries in a population it is most sensible to look for nephrotoxic agents the population might have been exposed to.
Since the increases coincide with the onset of the COVID-19 pandemic, experimental COVID therapeutics would be the main suspects.
We know Remdesivir probably contributes to what we are seeing, but maybe there are other drugs that do their part.
Other nephrotoxic COVID therapeutics
The WHO’s pharmacovigilance database “VigiBase” is not free. Why would it be when the WHO had been financed by German taxes for decades, right?
Always being broke, I never tried to gain access, but if I had, I would have probably not been approved after a careful review would have come to the conclusion that I am either anti-medicine, anti-science, anti-reason, anti-human or all of the above.
So instead I have to resort to VAERS reports.
VAERS Reports
I last updated my local VAERS database in late January, 2023, so it is a bit out of date. I performed a search for US reports including “COVID-19” in the SYMPTOMS field which yielded 98,349 results. Further limiting the query to reports with “Acute kidney injury” yields 1,633 results, while excluding “Acute kidney injuries” yields 96,716 results.
So now I can query both samples for mentions of drugs commonly used to treat COVID.
I browsed the reports for a few minutes to look for some candidates and ended up picking Remdesivir, Azithromycin, Ceftriaxone, Dexamethason and combinations of those terms.
These are the results:
You can see that the risk ratios (RR) are astronomically high, especially for Cetriaxone and and multiple drugs.
Experimental Pharmacotherapies
While there are probably more drugs involved in this large-scale poisoning of humanity, these are the four I picked for the query above:
Azithromycin (antibiotic)
Ceftriaxone (antibiotic)
Dexamethasone (corticoid)
Remdesivir (antiviral)
Azithromycin
Azithromycin is a popular macrolid antibiotic not generally considered nephrotoxic, but there have been reports of azithromycin-associated nephrotoxicity:
Ceftriaxone
Ceftriaxone seems to be among those antibiotics well-known to cause kidney stones and AKI (Source).
Dexamethasone
Some studies claim nephrotoxic properties:
Dexamethasone induced glomerular damage, proteinuria, renal oxidative stress and upregulated the renal Wnt/β-arrestin2/β-catenin pathway and the profibrotic signals. Blocking the α1 and βARs by carvedilol reduced the dexamethasone-induced nephrotoxicity. (Source)
Others attest the opposite effect in certain scenarios:
In summary, in the setting of renal ischemia-reperfusion injury, dexamethasone directly protects against kidney injury by a receptor-dependent, nongenomic mechanism. (Source)
Compared with sepsis group, the histopathological changes in the kidney were mitigated with different levels in groups treated with different doses of DEX (Source)
Remdesivir
At this point it is safe to assume that Remdesivir can generally be considered nephrotoxic. I’d assume its use in patients requires careful consideration of the potential benefits and tight monitoring of patients.
Not every doctor will be aware of this since there are coordinated efforts by rogue scientists to hide the truth. There seem to be entire networks of fake studies, letters and reviews that only serve to deceive. Here is a good examples for Remdesivir, that might make you chuckle:
Really? Let’s not go into this any further. This is just embarassing. Who would put their name on that?
We need a way to defame these scientists through a scoring system, so they think twice before publishing junk articles like these.
Conflicting information
This is a good article that illustrates why we don’t just label substances nephrotoxic and then avoid their use altogether: The 6R’s of drug induced nephrotoxicity
Interestingly enough it also mentions “the most common drugs that cause DIKD [Drug-Induced Kidney Injury] include antibiotics, […] antiviral agents”.
For every study about the nephrotoxic properties of any given drug you’ll find another that attests some type of benefit for renal function. There can be various reasons for this. In some cases the studies and conclusions drawn from them may be perfectly valid, but the toxicity or beneficial effects elicited by the substances in question are highly situational. In other cases, we are simply reading a product of scientific fraud.
Dosis (sola) facit venenum
“Dosis sola facit venenum” translates to “Only the dosage makes a poison”. Paracelsus, a radically revolutionary doctor who lived in the early 16th century, has famously written these words in his “Third Defense” (German text).
I warmly recommend reading this text for its entertainment value, if you happen to speak German or can find a good translation.
Whenever I quote him I skip the word “sola”, because it is not just the dosage that makes the poison.
It’s also the patient that makes a poison and the current state he finds himself in.
Genetic variation has a very strong impact on the activity and function of various enzymes, which can explain a drug’s variance in half-life, efficacy and toxicity between individuals
Genetic variation also leads to differences in receptor proteins, that can influence the binding profile of a drug
Drugs the patient is taking might be inducing or inhibiting enzymes critical for the metabolism of other drugs, but there is a nearly infinite number of mechanisms by which drugs can modulate each other’s effects when taken together. For example methanol poisoning turns intravenous ethanol into a lifesaving drug.
Stress can lead to temporary changes in how receptor proteins are expressed and assembled. In the case of Ethanol and GABA-A this can turn a generally sedating substance into one that is primarily excitatory (paradoxical reaction)
Disturbances in hormonal balance or nutritional deficits can turn substances into lifesavers, that would otherwise be detrimental to a healthy person’s life
Diseases often turn out to be caused by more than one pathogenic pathway, causing the same drug to be effective in one patient, but not in another, despite both presenting with the same symptoms.
Pregnancy, recent infections and even lack of sleep can all have profound effects on how a person reacts to a certain drug.
Age, gender and bodyweight are important factors that should nearly always be considered, regardless of which drug is being administered.
Is the patient running a fever? How well-hydrated is he? How much muscle mass does he have? Is he experiencing a lot of oxidative stress? The list goes on and on…
Many insights can only be gained from talking to the patient. Patient anamnesis is losing in importance in the hectic days of commercialized medicine and valuable information is often missed because of this.
One Size Never Fits All
The more data you have about a person and the more educated you are about outcomes in other patients that share features with the one you intend to treat, the better you can make an educated decision about what drugs you are going to administer and at what dosage.
Start recommending universal treatments, without any regard for all the things I mentioned above and you will end up poisoning people.
I think this is precisely what we are seeing.
The Great Poisoning that has probably already caused millions of deaths by kidney failure worldwide is the result of “One-Size-Fits-All-Medicine”.





























I have an alternate view on lung physiology that dismisses the notion of oxygen and carbon dioxide gaseous exchange
The article is titled
We breathe air not oxygen
I take you though all the steps that lead to this statement
Including how oxygen is manufactured
How oxygen is calibrated
Eg medical oxygen has 67parts per million of water contamination
Why oxygen is toxic, dehydrates and damages the alveoli
Lung physiology requires the air at the alveoli to reach 100% humidity
Can you see the problem?
The new take on lung physiology:
The lungs rehydrate the passing RBCs with iso tonic saline solution as they pass through the alveoli capillary beds
RBCs change from dark contracted dehydrated to plump bright hydrated form as they soak up the iso tonic saline solution the bursting alveoli bubbles throw upon the capillary sac
The airway mucosa conditions the breathe with salt and moisture
Find the article
Jane333.Substack.com
Well done.