Removing myocarditis reports for a new estimate
800,000 heart injuries among US children in the week after dose 2
Summary
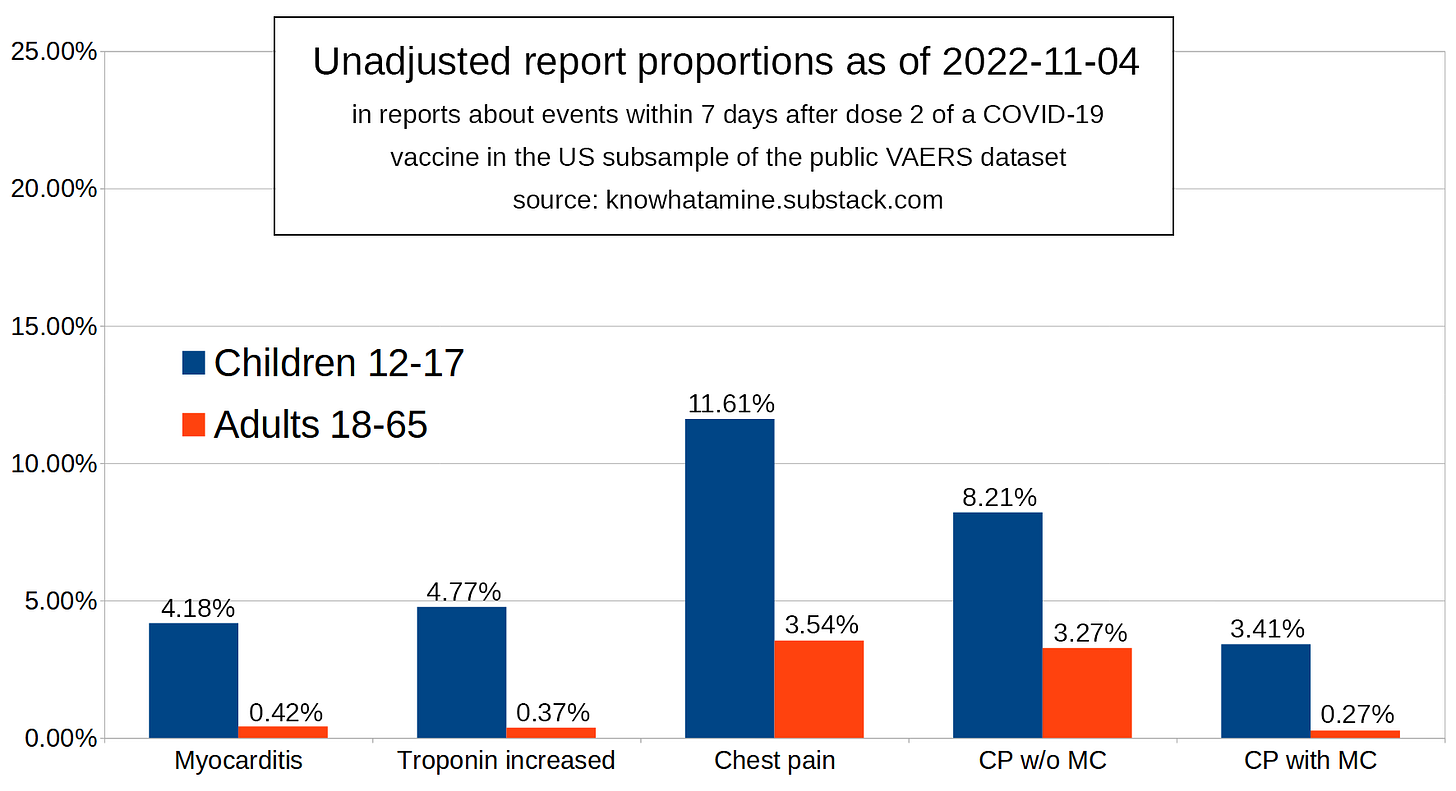
In my first article on this topic I estimated that 1 million children’s hearts were injured by the COVID-19 modRNA vaccines in the first week after they received their second dose.
In this article I am going to refine this estimate by assuming that myocarditis cases are overrepresented in the public VAERS dataset, due to the condition receiving a lot of media attention.
Removing 80% of myocarditis cases results in a lower estimate of a 6.19% for the incidence proportion within a week of receiving the 2nd dose, which brings our estimate of the number of childrens’ hearts that were injured this way to 800,000 in the USA alone.
Introduction
When looking at the difference between incidence proportion of myocarditis and the report proportion containing the term “Myocarditis”, we have to think about what is required for a case to be reported:
Syndrome needs to develop
Patient or doctor needs to report the adverse event
Each of these steps happens with an unknown probability. The type of medical concept in question affects these probabilities:
Some events are more often misdiagnosed than others (3)
Some diagnoses are reported with a higher probability than others due to raised awareness (4)
In the case of chest pain, headache, chills or fever less steps are required:
Symptom needs to be present
Patient needs to go see the doctor
Patient or doctor needs to report the adverse event
Since awareness has been raised among patients and doctors alike about myocarditis being a side effect of the modRNA injections, it can be assumed that a diagnosis being made strongly increases the chance of a report being made, similar to what can be seen in Herpes zoster, which report proportion is higher than its incidence proportion.
However when chest pain occurs as an isolated symptom absent of a diagnosis for myocarditis, its occurence alone should not increase the chance of the event being reported compared to other isolated or co-reported symptoms.
Similarly, when chest pain accompanies other unrelated diagnoses (e.g. bell’s palsy, anosmia, pulonary embolism), we assume it is not more likely to find its way into a report than comparable symptoms, like headache or fever.
So in order to refine the model and our resulting estimate, I am making an adjustment.
Methods
I will be applying the same methods as I did reaching my initial estimate, but will separate the reports for chest pain into two groups before we begin:
Reports mentioning both chest pain and myocarditis
Reports mentioning chest pain, but not myocarditis
Keep in mind that a term that is overrepresented can still be underdiagnosed and underreported, just less so than adverse events are generally underreported. All the term “overrepresentation” means in this context is that the incidence proportion of the diagnosis is lower than the report proportion.
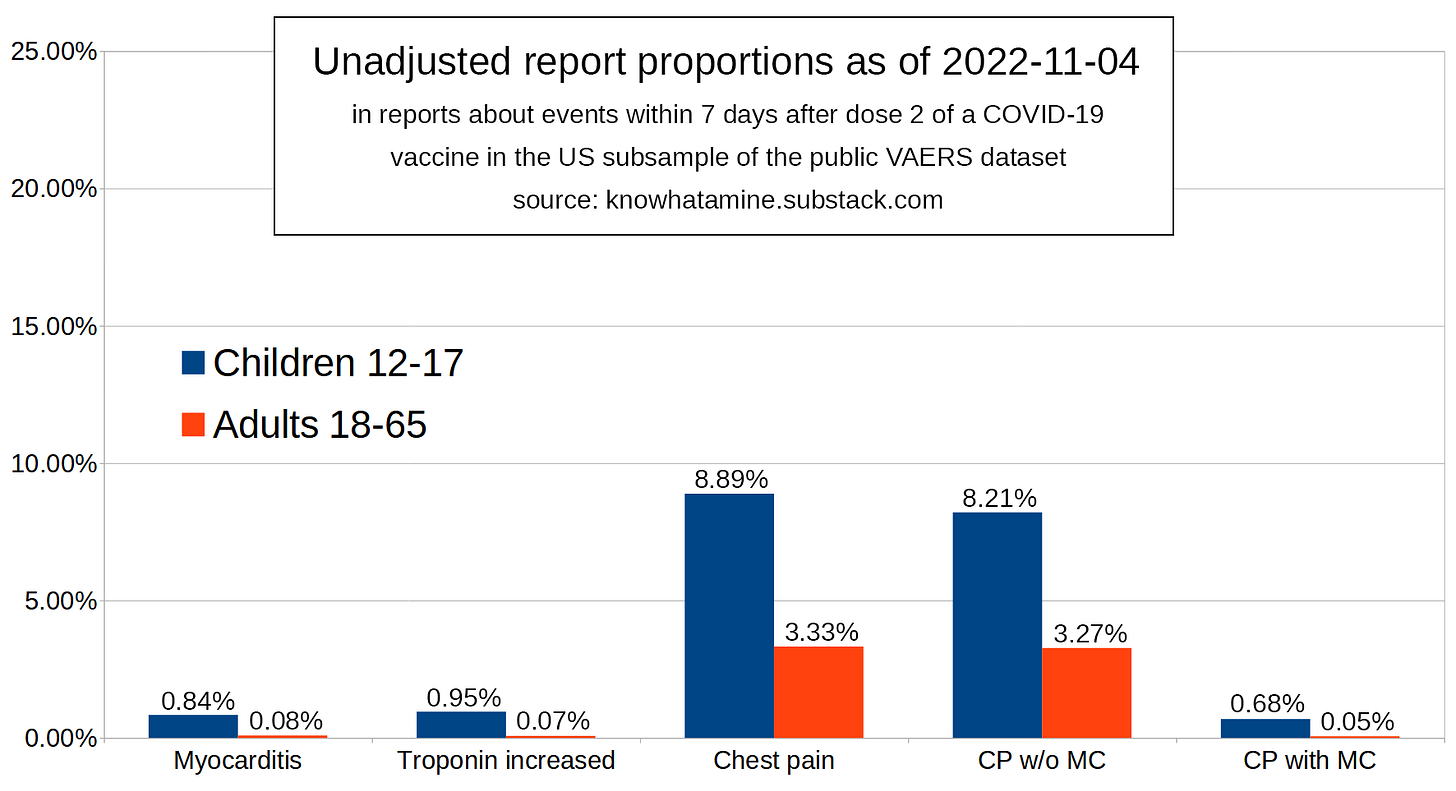
Therefore I will generously assume an overrepresentation factor of 5 for “Myocarditis”, similar to the overrepresentation factor of “Herpes zoster” (4.4). This factor will be applied to the proportion of chest pain reports that also mention “Myocarditis”.
I will keep assuming all remaining mentions of “Chest pain” are equiproportionally represented, much like the terms “Headache”, “Chills” or “Pyrexia”. Therefore we will add the reduced proportion of “Chest pain” reports that mention “Myocarditis” to the unchanged proportion of “Chest pain” reports that do not mention “Myocarditis” and apply this report proportion as if it were an incident proportion to the total number of children double-dosed with a modRNA vaccine.
Results
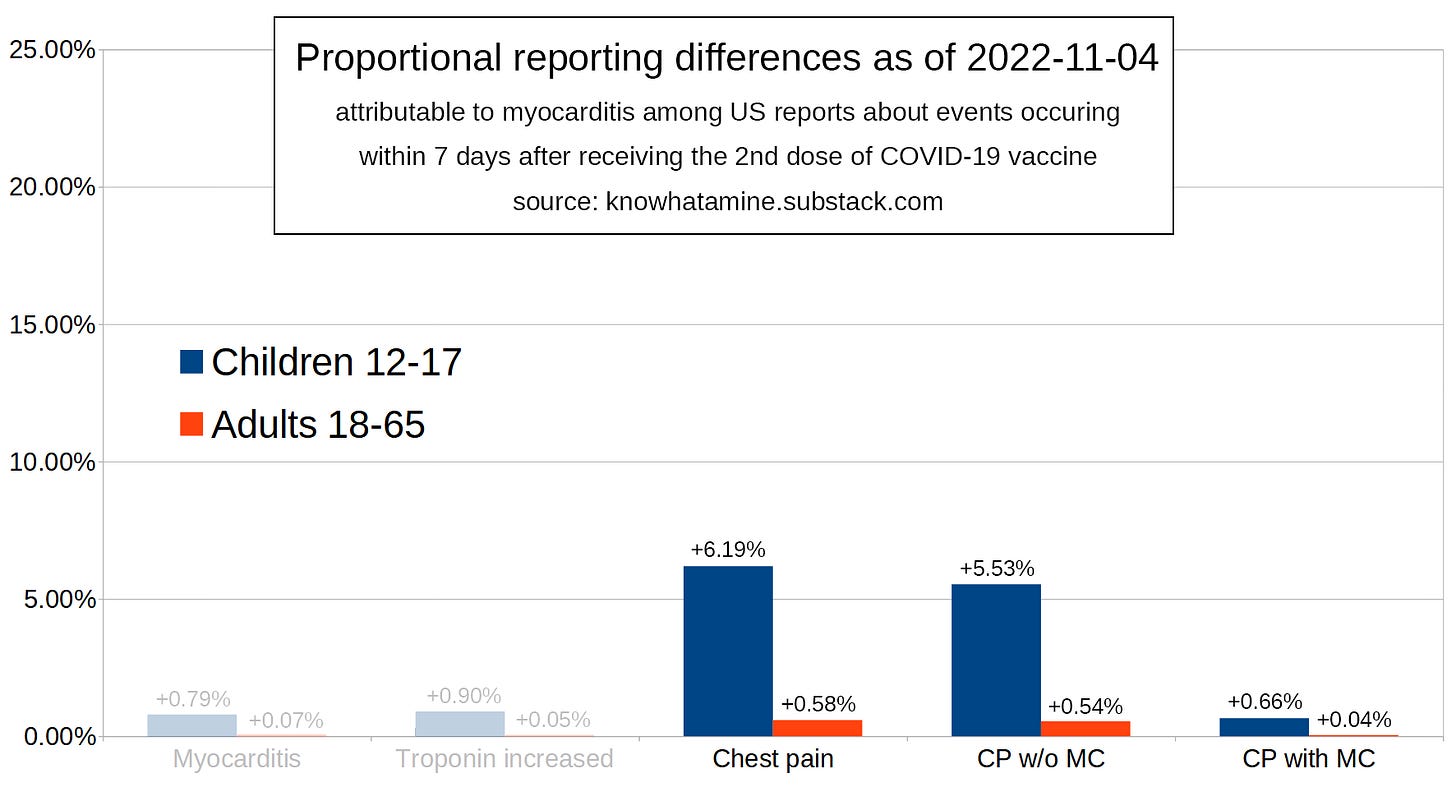
This time we are going to divide the proportion of “Chest pain” occurences co-reported with “Myocarditis” by 5, removing 80% of these events:
This is our reference group. The proportions are subtracted from the report group’s proportions in our study group to remove misattributed events.
Now we are our looking for the proportion of “Chest pain” events that has the correct ratio of child/adult proportions in events of chest pain without myocarditis.
This reduces the proportions from 6.82% and 1.85% to 5.53% and 0.54% respectively. Now we are adding to that the remaining 20% of myocarditis-associated chest pain reports:
The resulting report proportion of children who spontaneously reported chest pain that is presumably attributable to heart injury is 6.19%. If we assume equiproportional representation for these symptoms we can calculate the total number of heart injuries using our knowledge about the total number of American children aged 12-17 that were double-dosed:
x = n * p = 15100000 * 0.0619 = 934,690
x = n * p * URF_2_7 = 7,104 * 6.19% * 1475 = 648,612
Discussion
Everything I did had already been explained in previous articles or inside the introduction to this article.
However there is something else I’d like to point out. The authors of the Polish study claim:
“In addition, having earlier suffered from COVID-19 had an impact on the occurrence of more severe side effects after the first dose of the COVID-19 vaccine.”
This makes me wonder: Seeing that the report proportion of myocarditis increases by around 10% in individuals who are said to have been infected with SARS-COV-2, regardless of the number of doses they took, is there a chance that only those who were exposed to SARS-COV-2 develop myocarditis after round 1 of the vaccine?
Could that be the reason why we saw many less myocarditis cases in Pfizer’s phase III trials in adults than we would have expected to see with knowledge of the data we have now?
Conclusion
Since both models are still flawed and we will probably refine them further in the future we will just settle for the middle ground as our best bet for now:
800,000 injured hearts




At a small conference in Austria, 2021, the cardiologists discussed that they had been keeping their own estimates for injury following the shot. They had a one in six rate for boys, but said it was possible that everyone who took it had heart injury and simply didn't recognize the symptoms - you don't go to the doctor it it's harder climbing up stairs. They weren't sure what was happening in girls because the patients coming in were predominantly male and the standard tests weren't giving clear signals on females. I trust their experience, and it makes sense from a cell biology perspective.
(Edit: thanks for another great article!)